1. Introduction to Laser Phototherapy
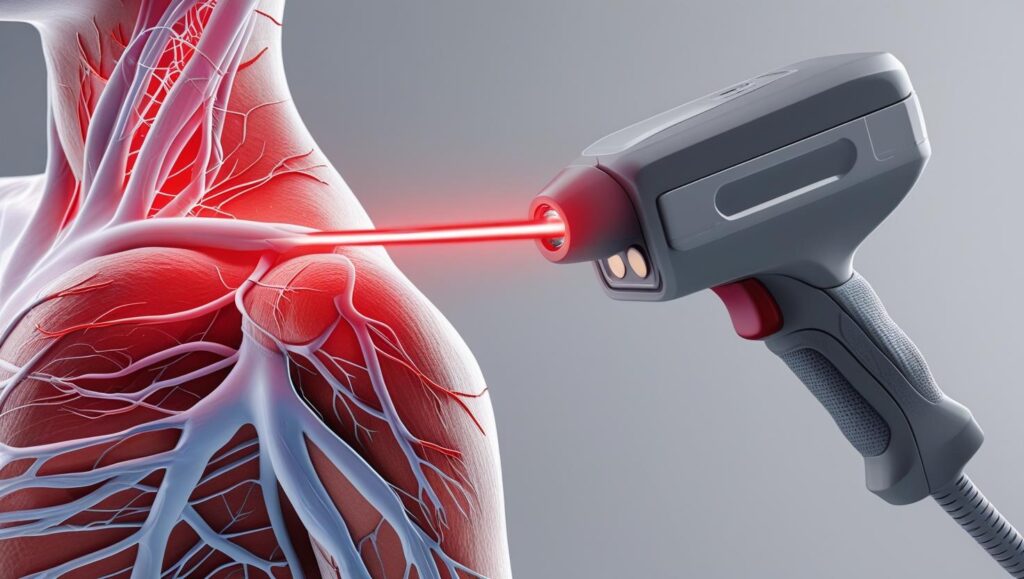
Laser ptotherapy, also known as low-level laser therapy (LLLT) or photobiomodulation (PBM), involves the application of low-intensity laser or light-emitting diode (LED) light to stimulate biological processes in tissues. Unlike high-power surgical lasers that cut or ablate tissue, phototherapy uses non-thermal, non-destructive light to enhance cellular function, reduce inflammation, and promote healing.
Key Characteristics of Laser Phototherapy:
- Non-invasive – No tissue damage or surgical intervention required.
- Painless – Patients typically feel no sensation during treatment.
- Versatile – Used across multiple medical specialties.
- Minimal side effects – Safe when used correctly.
2. Historical Development of Laser Phototherapy
The therapeutic use of light dates back to ancient civilizations, but modern laser phototherapy began with the invention of the laser in 1960.
Milestones in Laser Phototherapy:
- 1960 – Theodore Maiman develops the first working ruby laser.
- 1967 – Endre Mester discovers “laser biostimulation” while studying laser effects on cancer in mice.
- 1980s-1990s – Clinical adoption expands in dentistry, dermatology, and physical therapy.
- 2000s – Introduction of LEDs and advancements in photodynamic therapy (PDT).
- 2010s-Present – Standardization of protocols and FDA approvals for various indications.
3. Basic Principles of Laser-Tissue Interaction
Laser phototherapy works through photochemical and photobiological effects rather than thermal damage. Key principles include:
Photobiomodulation (PBM) Mechanism:
- Photon Absorption – Light is absorbed by mitochondrial chromophores (cytochrome c oxidase).
- Cellular Response – Increased ATP production, reactive oxygen species (ROS) modulation, and nitric oxide release.
- Therapeutic Effects – Reduced inflammation, enhanced tissue repair, and pain relief.
Parameters Influencing Efficacy:
- Wavelength (600-1000 nm for deep penetration)
- Power Density (mW/cm²)
- Energy Density (J/cm²)
- Pulse Frequency (Continuous vs. Pulsed)
4. Types of Lasers Used in Phototherapy
Different lasers are chosen based on penetration depth and target tissue.
| Laser Type | Wavelength (nm) | Clinical Uses |
|---|---|---|
| Helium-Neon (He-Ne) | 632.8 | Wound healing, dermatology |
| Diode Lasers | 630-980 | Pain relief, dentistry, musculoskeletal |
| Nd:YAG | 1064 | Deep tissue therapy, vascular lesions |
| Erbium (Er:YAG) | 2940 | Skin resurfacing, dental procedures |
| KTP Lasers | 532 | Vascular lesions, pigmentation treatment |
5. Mechanisms of Action in Laser Phototherapy
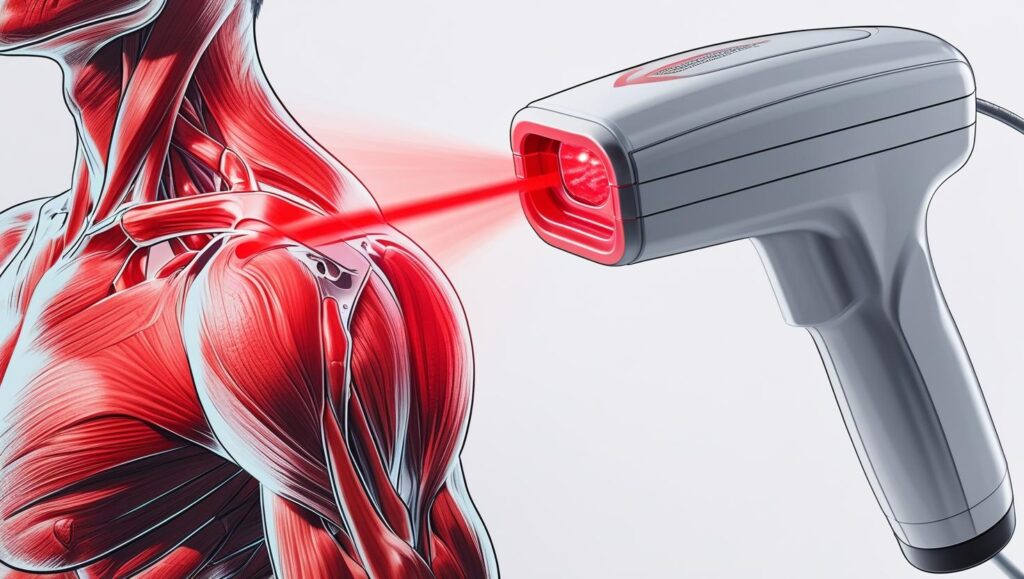
Biological Effects:
- Anti-inflammatory – Reduces pro-inflammatory cytokines (IL-6, TNF-α).
- Analgesic – Modulates nerve conduction and endorphin release.
- Regenerative – Stimulates fibroblast proliferation and collagen synthesis.
- Angiogenic – Promotes new blood vessel formation.
Cellular Pathways:
- Mitochondrial Activation ↑ ATP synthesis.
- NF-κB Pathway Modulation ↓ Inflammation.
- TGF-β Stimulation ↑ Tissue repair.
6. Clinical Applications of Laser Phototherapy
A. Dermatology & Aesthetic Medicine
- Acne Treatment – Reduces P. acnes bacteria and inflammation.
- Psoriasis & Eczema – Decreases plaques and itching.
- Hair Regrowth – Stimulates follicles in androgenetic alopecia.
- Scar Reduction – Improves collagen remodeling.
- Skin Rejuvenation – Enhances elastin and reduces wrinkles.
B. Pain Management & Musculoskeletal Disorders
- Osteoarthritis – Reduces joint pain and stiffness.
- Tendinopathies (e.g., tennis elbow, Achilles tendinitis).
- Myofascial Pain Syndrome – Relaxes trigger points.
- Fibromyalgia – Alleviates widespread pain.
C. Wound Healing & Tissue Repair
- Diabetic Ulcers – Accelerates healing in chronic wounds.
- Burns – Reduces healing time and scarring.
- Post-Surgical Recovery – Enhances tissue regeneration.
D. Dentistry & Oral Medicine
- Periodontitis – Reduces gum inflammation.
- Tooth Sensitivity – Seals dentinal tubules.
- TMJ Disorders – Relieves jaw pain.
- Oral Mucositis (e.g., from chemotherapy).
E. Ophthalmology
- Macular Degeneration – Slows progression (experimental).
- Dry Eye Syndrome – Improves tear production.
F. Neurology & Rehabilitation
- Peripheral Neuropathy – Improves nerve function.
- Stroke Rehabilitation – Enhances motor recovery.
- Spinal Cord Injury – Promotes axonal regeneration.
G. Oncology (Photodynamic Therapy – PDT)
- Cancer Treatment – Uses photosensitizers (e.g., 5-ALA) to destroy tumors.
- Actinic Keratosis & Basal Cell Carcinoma – Non-surgical ablation.
H. Veterinary Medicine
- Osteoarthritis in Pets – Pain relief in dogs and horses.
- Wound Healing in Animals – Post-surgical recovery.
7. Treatment Protocols and Dosimetry
Key Parameters:
- Dose (J/cm²) – Typically 1-10 J/cm² depending on condition.
- Frequency – Acute conditions: Daily; Chronic: 2-3x/week.
- Duration – 30 sec to 10 min per session.
Common Treatment Modalities:
- Contact vs. Non-contact Application
- Grid Technique for Large Areas
- Intraoral Probes in Dentistry
8. Safety Considerations and Contraindications
Side Effects (Rare):
- Mild erythema, temporary discomfort
9. Future Directions and Innovations
- Nanoparticle-Enhanced Phototherapy
- Personalized Wavelength Selection
- Wearable Laser Devices
10. Conclusion
Laser phototherapy is a versatile, evidence-based modality with applications across multiple medical fields. Ongoing research continues to expand its therapeutic potential, making it an essential tool in modern medicine.